We found 53 results for EFM

EFM Advanced #01: Terms & Guidelines Part 1
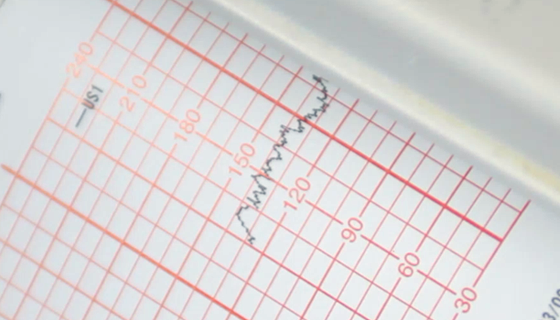
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the first of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
EFM Advanced #02: Terms & Guidelines Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the second of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
EFM Advanced #03: Physiology & Pathophysiology Part 1
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the third of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #04: Physiology & Pathophysiology Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the fourth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #05: Interventions & Management Part 1
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the fifth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #06: Interventions & Management Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the sixth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #07: Interventions & Management Part 3
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the seventh of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #08: Interventions & Management Part 4
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the final of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #01: OP Malpresentation
In an effort to reduce cesarean births due to fetal malpresentation, ACOG encourages practitioners to perform manual rotation of the fetal occiput in the setting of fetal malposition in the second stage of labor as an intervention prior to operative vaginal delivery or surgery. This activity explores through case studies the various interventions for patients with OP malpresentation.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #02: EFM Triage, Part 1
This activity provides an EFM triage model for swift and accurate EFM interpretation when there is no clinical information about the mother or her pregnancy.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #02: EFM Triage, Part 2
This activity provides practice using an EFM Triage model for swift and accurate EFM interpretation when there is no clinical information about the mother or her pregnancy.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #03: Standard Terms and Guidelines
Utilization of standardized electronic fetal monitoring (EFM) nomenclature nationwide remains inconsistent from hospital to hospital and practitioner to practitioner. This activity outlines how to apply standardized EFM nomenclature, 3-Tier FHR Interpretation System and the ACOG intrapartum management algorithms into clinical practice in a case study format. EFM risk management concerns are defined.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #04: Neonatal Encephalopathy
New guidelines outlined in the ACOG & AAP Task Force Report on Neonatal Encephalopathy (NE) include scientific updates on specific fetal heart rate patterns, sentinel events, and newborn assessment indicators that may indicate an acute intrapartum hypoxic-ischemic injury that leads to NE or cerebral palsy. This activity reviews the new guidelines in a case study format to improve application.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #05: pH Implications
Umbilical cord blood sampling is used to determine if the cause of neonatal encephalopathy or cerebral palsy is linked to a peripartum or intrapartum event. Critical values are defined by ACOG & AAP. This activity presents an overview of oxygen delivery, definitions of critical values, and analysis of EFM strips for pH interpretation in a case study format.
.png?access_token=3003rOZj405nAWK74EDMD06eU9vefmkwOOi5kdKz)
EFM Case Study #06: Oxygen Therapy Update
Both hyper- and hypoxemia can have a negative impact on a fetus and neonate. Current scientific evidence and clinical guidelines support low dose and short duration maternal oxygen therapy during intrapartum.
We found 3 results for EFM
-
Education
Section: MI Public Website -
Assessments
Section: MI Public Website -
Course Packages
Section: MI Public Website

